Answer of Dermatopathology Case 100
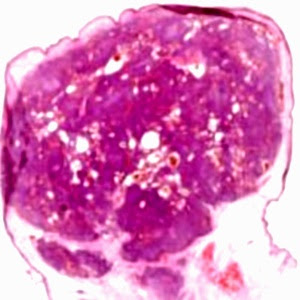
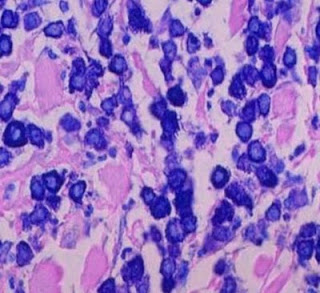
Retiform Hemangioendothelioma Visit: Dermatopathology Site Visit: Pathology of Hemangioendothelioma Abstract: Retiform haemangioendothelioma: a case report.Ann Pathol. 2009;29(6):491-4. Retiform haemangioendothelioma is a locally aggressive, very rarely metastasizing vascular lesion. Histologically, it is characterized by distinctive arborizing blood vessels resembling "rete testis" and lined by endothelial cells with characteristic hobnail morphology. We present an additional case, in the leg of a 64-year-old patient. We discuss the classification of hemangioendotheliomas. The term hemangioendothelioma should be restricted to vascular tumours of "intermediate malignancy" but has been used to designate tumours with variable histological features and clinical behaviour. Spindle cell hemangio(endothelio)ma is currently regarded as a benign reactive lesion. Kaposiform hemangioendothelioma is potentially lethal due to consumption coagulopathy but no metastasizing case h