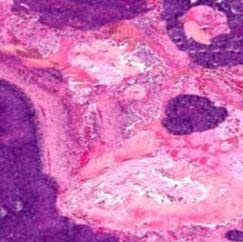
Answer of Dermatopathology Case 28
Molluscum Contagiosum Visit: Molluscum Contagiosum Visit: Dermatopathology site Visit: Infectious Disease Online Abstract: Mollusca contagiosa. From paediatric dermatology to sexually transmitted infection.Hautarzt. 2009 Jun;60(6):472-6. Molluscum contagiosum (MC) is a common cutaneous infection caused by the molluscipox virus (MCV) and can affect both children and adults. Molluscum contagiosum is relatively frequent in children aged 1-5 years old and can be localized almost anywhere on the body, but in adults it is regarded as a sexually transmitted infection (STI). MCV can be transmitted directly from person to person or by autoinoculation. MC in adults characteristically involves the genital area but extragenital appearance can be more typically seen in patients with immunosuppressive conditions, especially in HIV/AIDS. The onset of MC inHIV-positive individuals can be regarded as a part of the immune reconstitution inflammatory syndrome (IRIS). MC probably affects both sexes equall...